Unless you’ve been directly affected by it, chances are you have no idea what Pulmonary Arterial Hypertension is. From the name, you can probably work out that it has to do with the Pulmonary (Respiratory) System, but that’s normally where the understanding ends. With this blog, I hope to raise awareness for. PAH, connect with others and share what it’s like to be a Rare Disease Caregiver.
A little background
As a caregiver for the last 14 years, I’ve become intimately acquainted with this awful disease. I’ve spent nearly 5,000 hours caring for my wife and learning everything I could about PAH. I’ve compounded IV drugs, performed injections and helped maintain her life-saving equipment. I’ve helped administer and track nearly 80,000 pills, gone to all but two of her weekly blood work and bandage changes, and accompanied her on over 1,000 medical appointments and tests. I’ve also been by her side for ever hospitalization and ICU stay aside from a short stint in 2022 when COVID prevented me from entering her room. I’m no medical professional, but I have gained a great deal of knowledge about this disease and I hope to share it with you.
What is Pulmonary Hypertension?
Pulmonary Hypertension, PH for short, is just a general term or phrase used to describe to the condition of high blood pressure in the lungs. When we hear the word Hypertension we often think of systemic hypertension, or the ‘high blood pressure’ that affects the whole body and can be measure with a blood pressure cuff around the arm. Pulmonary Hypertension is similar, except that the high blood pressure is concentrated in the lungs. Unlike regular high blood pressure, PH can’t be easily detected with a blood pressure cuff. It requires advanced imaging through echo cardiograms, right-heart catheterizations and sometimes additional procedures in order to identify the type of PH and it’s extent.
Most often PH remains hidden, progressing significantly but silently over time until it’s symptoms become severe and the disease itself quite advanced. The condition of PH can be attributed to a variety of sources and likewise, can present itself in a several different forms. Sometimes we tend to think of diseases in stages, i.e. Stage 2 Breast Cancer as an example. But PH is a little different.
The Types of Pulmonary Hypertension
There are five main types of Pulmonary Hypertension which refer to the cause or the origin of the condition. Sometimes they are called groups instead of types, i.e. WHO Group 1 Pulmonary Hypertension, due to how the World Health Organization originally classified patients with PH. I found this little comic on medcomic.com, and I really like it (link goes to original source):
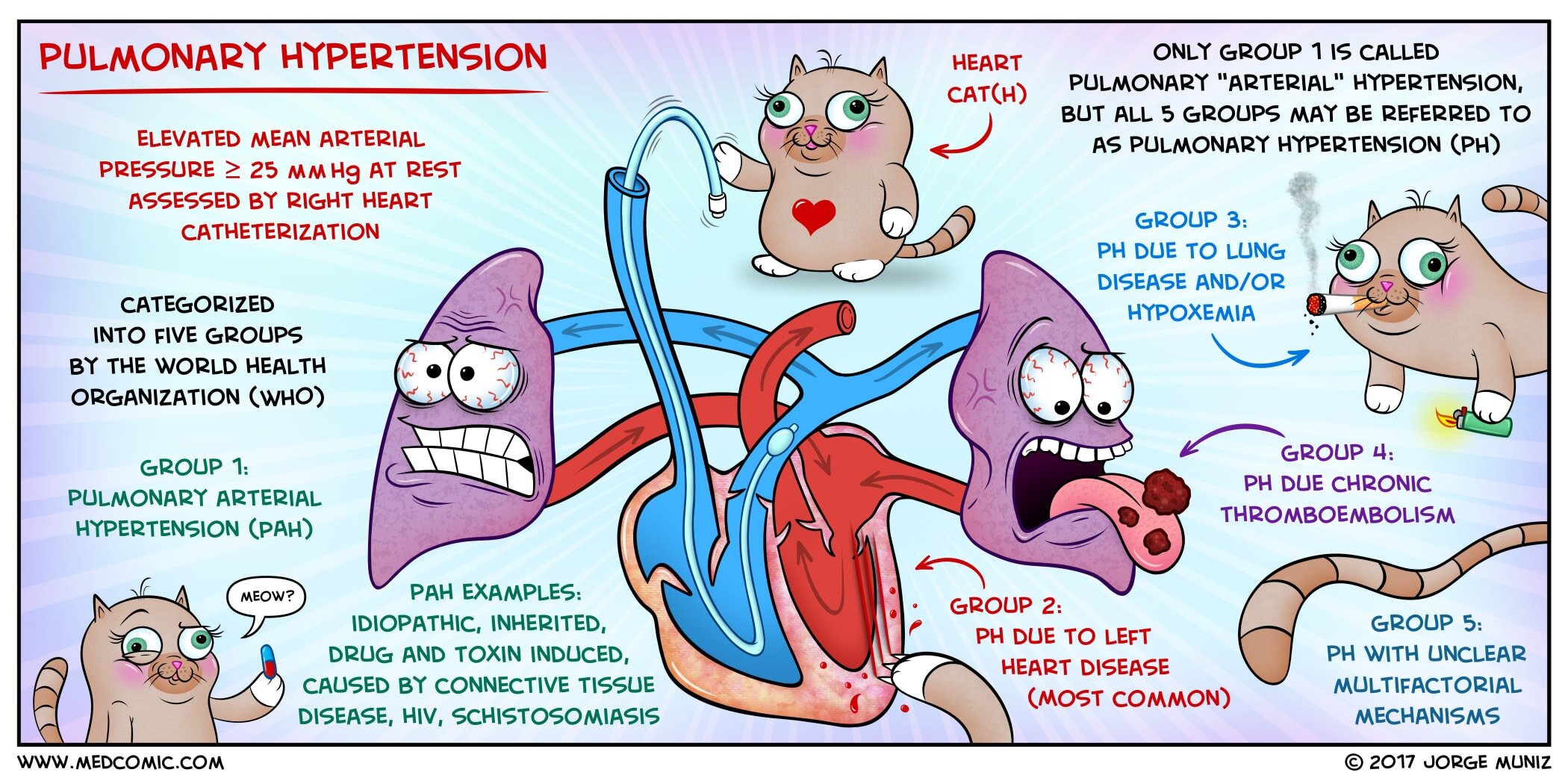
WHO Group 1 refers to Pulmonary Arterial Hypertension, the kind my wife has. It can be Idiopathic (IPAH as in my wife’s case with no evident cause), Heritable (linked to, but not directly caused by certain genes the patient shares with family members), or it can occur as a result of something else like STD’s, certain types of drug use and even old diet pills from the 1980’s (FEN FEN anyone?).
When my wife was diagnosed, we were told she was the ‘poster child’ for WHO Group 1 PH or IPAH; the worst form. Severe, incurable and rapidly progressing with no evident source and limited treatment options that all ended up at a lung transplant. Subsequent genetic testing would show the presence of the mutated BMPR2 gene, though it appears to be random and not passed down from her parents. She’s one unlucky lady, my wife.
WHO Group 2 refers to PH that is caused by left-heart disease. It’s the most common form and it happens when the heart is weakened and works too hard.
WHO Group 3 refers to PH caused by lung diseases such as COPD, emphysema, sleep apnea, interstitial lung disorder or pulmonary fibrosis.
WHO Group 4 is PH from a specific lung condition called CTEPH, and this type of PH can potentially be cured by surgical intervention.
And finally, WHO Group 5 is simply PH with no known source. It could occur after an organ removal surgery or in conjunction with certain types of anemia.
Whats really going on in the lungs?
That’s the question I had to find out. So, pamphlet in hand from my wife’s Pulmonologist, I went straight to the PH Association and I dug in. For patients with PAH, the arteries and blood vessels in the lungs become thick and rigid. These vital pathways begin to narrow and develop scar tissue that impedes the circulation. The right side of the heart (the smaller/weaker side), is unable to get enough blood into the lungs where it can pick up oxygen and then be pumped out to the body through the left side of heart (the bigger/stronger side).
As a result, PAH patients often are starved for oxygen and rapidly descend into right-heart failure. The smaller right side gets backed up and the muscle works itself to failure. Imagine standing on the hose of a water pump and watching the engine fail, that’s essentially what happens to a PAH patient. Instead of the stronger left-heart breaking down over time due to heart disease, the weaker right-heart fails due to the lung disease.
Patients like my wife Jennifer are often fatigued, out of breath and have chest pains due to low oxygen, poor circulation and the heart failure that come along with it.
The PH Association of America
I’d be remiss not to say a few words about The Pulmonary Hypertension Association of America. The PH Association is the foremost charitable organization for the advancement of treatment options, education and awareness for all forms of PH. The site is linked here, and as someone who has consistently turned to the PH Association for everything from education to advocacy efforts, to caregiver support, I cannot recommend them highly enough. I go there first and always for information and to donate to! You should too!
So how do you treat PAH?
Great question. It was the most pressing question that my wife and I had, and it’s one we’ll have for the rest of our lives. We have been fortunate to see two new therapies be approved in the last decade, both of which have the potential to greatly extend and improve the quality of life for PH patients, OPSUMIT and WINREVAIR. There have been others as well, I list these two as they are the ones I’m familiar with as a caregiver, and my wife is familiar with as a patient. While it will never be a good time to have PH or PAH, we live in a time of tremendous hope. And hope is the only medication we’ve seen, that doesn’t have a bad side effect.
Forty years ago, PH was little more than a rapid death sentence with virtually no treatment options. Thirty years ago there were one or two treatment options which were promising and being prescribed, but there was a lack of solid data. When my wife was diagnosed 14 years ago there were a few oral and IV treatment options, not to mention lung transplantation had steadily improved. And there was more data for the Doctors to use to determine which treatments to try on her. As her first Pulmonologists told us at diagnosis, more data is better data.
Today there are a number of treatment options from pills and inhaled treatments to 24/7 subcutaneous and IV options. In 2024, a new injectable called WINREVAIR was also approved and it has the potential to come as close to reversing the disease as we’ve ever seen. There is much to be hopeful about.
A typical PAH patient like my wife will tend to use a combination of PH-specific therapies in addition to blood thinners and diuretics. In her case, she uses the PH-specific drugs WINREVAIR, Remodulin IV, Opsumit, and Revatio (Viagra). Yes, you read that correctly, Viagra. Before the little blue pill became man’s best friend, it was actually developed and used to treat Pulmonary Hypertension, most often in women. Fancy that.
My wife also requires supplemental oxygen during exercise and when she sleeps, and she has to maintain a very strict diet which limits fluid and sodium intake. She looks like most women her age (way more beautiful), with the exception of a port in her chest which connects to a pump that delivers lifesaving IV medication 24/7 via six feet of tubing.
The hole in her chest is sometimes called a central line or a port and the long white tube hanging out of it is called a Hickman Catheter. Here’s a link for more information and here’s what a Hickman Catheter looks like in the wild, i.e. on my wife’s chest. I like to call it her boob tube:

See that little hole next to where the Hickman catheter is coming out? Her Hickman catheter used to come out from that one, until December 2024 when she got an infection. Now, she’s got an extra dent in her chest next to a fresh hole! It’s a little morbid, but we have to take humor where we can.
So what’s next?
Great question. We plan to blog on Newlungsplz few times a week, with topics and blogs split between my wife and I as patient and caregiver. We’ll video some of her IV meds and injections, as well as her daily and weekly tasks, exercises, etc. We hope to really use this blog to raise awareness for Pulmonary Arterial Hypertension, Rare Disease Caregiving and much more. We hope you join us on this journey!
Terry / PHind A Cure